Type 2 Diabetes: A Growing Global Challenge
Diabetes is no longer only a disease of the elderly. Today, more and more people under 40 are being diagnosed with type 2 diabetes.
According to The Lancet (2023), individuals diagnosed before the age of 30 may lose up to 14 years of life expectancy compared to their peers. Early-onset diabetes also means earlier and more severe complications, including kidney disease, vision loss, and cardiovascular problems.
Worldwide, an estimated 35% of adults are in a “pre-diabetes” stage. Without intervention, up to 64% of them will develop diabetes within five years.
The biggest driver behind this trend? Obesity and poor diet.
Obesity at a young age accelerates the incidence of type 2 diabetes.
According to the 2025 Lancet series of articles:
- Over the past 30 years, global obesity rates have surged by 244%, with adolescents and young adults being the hardest hit.
- A hospital-based study in China revealed that the prevalence of type 2 diabetes among individuals under 18 years old more than doubled, rising from 0.04 per 1,000 people in 1995 to 0.10 per 1,000 people in 2010.
Obesity is one of the primary causes of early-onset type 2 diabetes in adolescents. Data indicate that approximately 85% to 90% of adolescents diagnosed with type 2 diabetes are already obese at the time of diagnosis.
Beyond the notion of “not being able to control one’s appetite or get enough exercise,” researchers have introduced a new concept: the obesogenic environment.
What does that mean?
Gaining weight isn’t simply because you lack self-discipline or love food too much—it’s because this world itself is a bit “corrupt.” In this environment, it’s hard not to indulge.
For example—
- Food delivery at your beck and call, satisfying midnight cravings anytime;
- Group orders for bubble tea are cheaper than single cups, with endless discounts on snacks and desserts;
- Living spaces are shrinking while life speeds up relentlessly;
- Foods packed with more sugar and oil cause calories to skyrocket with just a bite.
A while back, a comparison video went viral on TikTok: The same snack in the U.S. had a significantly longer list of “weight-gain ingredients” on its label than the European version—high fructose corn syrup, hydrogenated vegetable oil, and corn syrup… It’s practically designed to make you fat.

Don't wait until symptoms appear to regret it—Type 2 diabetes can actually be stopped earlier.
Type 2 diabetes does not develop suddenly; it has a “reversible buffer zone”—prediabetes.
Pre-diabetes has no obvious symptoms, but the pancreas has already begun to malfunction. If blood sugar levels are controlled and weight is managed at this stage, the onset of diabetes may be delayed or even prevented. Even if it ultimately cannot be avoided, delaying its onset would still be a tremendous success.
Determining High-Risk Status
If you meet any of the following criteria, you are considered high-risk:
- Waist circumference exceeds standards (men >90cm, women >85cm)
- Family history of diabetes
- Fatty liver disease or polycystic ovary syndrome (PCOS)
- History of gestational diabetes
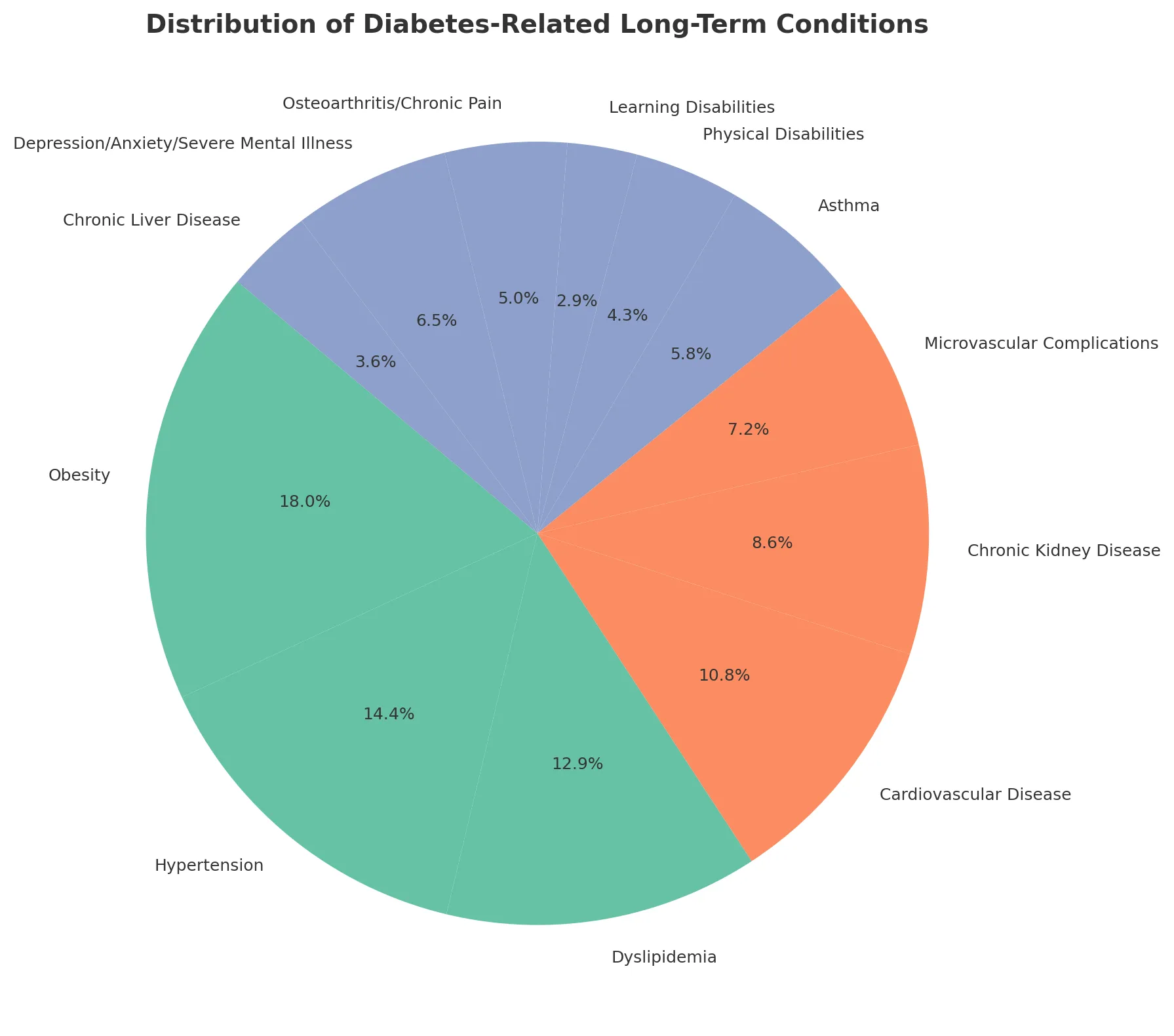
- Metabolic disorders such as hypertension or hyperlipidemia
- BMI exceeding 24 or abdominal obesity
- Sedentary lifestyle, frequent late nights, high stress, or frequent consumption of sugary drinks
- Recent sudden weight gain, excessive sleepiness, increased appetite,
- Persistent dry mouth or thirst
Regular blood sugar monitoring is recommended
You may visit the endocrinology department to have the following three indicators tested:
- Fasting blood glucose
- 2-hour postprandial blood glucose
- Glycated hemoglobin
Lose weight! Develop more healthy lifestyle habits!
For those at high risk and teetering on the edge—good news: you don’t necessarily need medication. Reversing the situation is possible through lifestyle changes alone!
Obesity and the accompanying blood sugar abnormalities are closely tied to lifestyle choices. The first step is adjusting your diet and exercise routine to break free from the unhealthy environment that fuels weight gain.
Why Diet Matters in Type 2 Diabetes Management
Blood sugar control is directly linked to the type of carbohydrates people eat. Highly processed foods, sugar-sweetened drinks, and refined flour products spike blood sugar quickly, making diabetes harder to manage.
On the other hand, foods that are low in calories, high in fiber, and rich in protein can help:
- Slow down sugar absorption.
- Improve satiety and reduce overeating.
- Support healthy weight management.
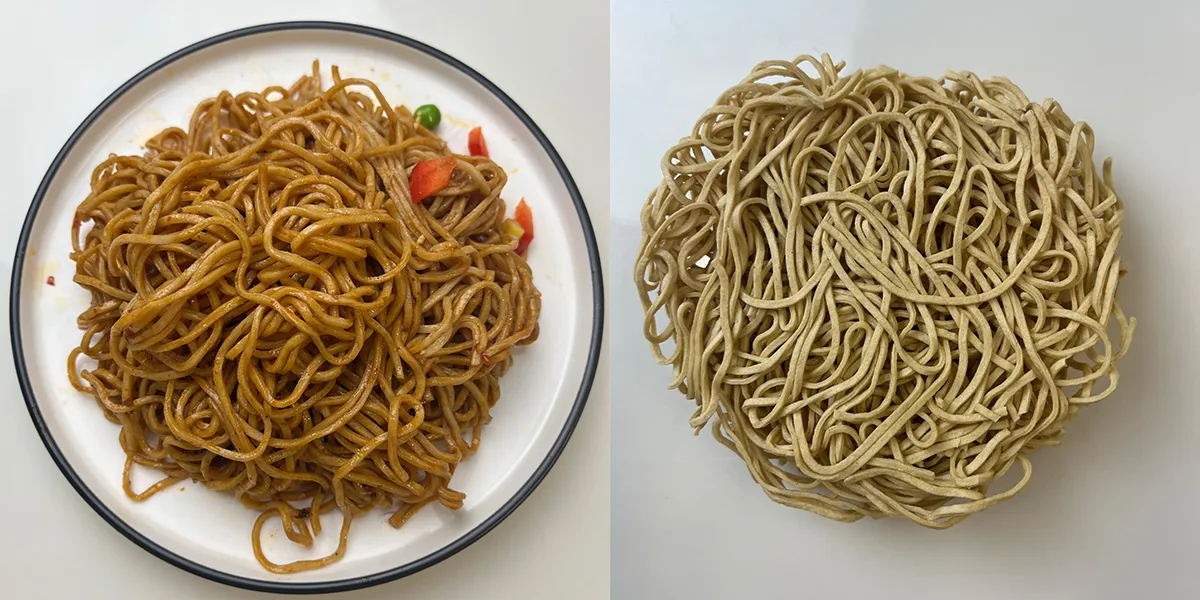
This is where Konjac noodles and High Protein noodles can play a role in everyday diets.
Konjac Noodles: Naturally Low-Carb and High-Fiber
Konjac (also called glucomannan) is a natural plant root widely used in Asia. Noodles made from konjac are:
- Very low in calories (about 10–15 kcal per 100 g).
- High in soluble fiber (glucomannan), which forms a gel in the stomach, slowing digestion and sugar absorption.
- Carb-friendly — almost no digestible carbohydrates.
A clinical review in Journal of Obesity (2020) found that glucomannan supplementation improved fasting blood sugar and reduced LDL cholesterol in people with type 2 diabetes. Another meta-analysis (Diabetes Research and Clinical Practice, 2021) confirmed its role in improving HbA1c levels.
Practical benefit: Eating Konjac noodles instead of refined wheat pasta or rice helps reduce overall calorie and carb intake without losing the feeling of fullness.

High Protein Noodles: Supporting Satiety and Muscle Health
Protein is essential for blood sugar control because it slows carbohydrate absorption and improves satiety. For people with diabetes, a higher-protein diet (20–30% of daily calories) has been linked to:
- Better blood glucose control (American Journal of Clinical Nutrition, 2019).
- Improved weight management.
- Maintenance of lean muscle mass, which is especially important as people age.
High Protein noodles are designed with added plant proteins, providing a convenient way to replace traditional carb-heavy meals with balanced nutrition.
Comparison of Regular Noodles vs. Diabetes-Friendly Options
Product | Calories (per 100 g) | Carbohydrates (g) | Fiber (g) | Protein (g) | Glycemic Impact |
Regular Wheat Noodles | 138 kcal | 25 g | 1 g | 4 g | High |
Konjac Noodles | 10–15 kcal | <1 g | 3–5 g | <1 g | Very Low |
High Protein Noodles | 120–150 kcal | 15–20 g | 3–4 g | 12–18 g | Moderate–Low |
Sources: USDA Database, Journal of Obesity (2020), Product Nutrition Labels.
Lifestyle + Smart Food Choices = Diabetes Prevention
Research shows that delaying diabetes diagnosis by 10 years can add 3–4 years of life expectancy (The Lancet, 2023). This means lifestyle and food choices really matter.
Tips for people at risk of diabetes:
- 1.Choose low-GI carbs such as Konjac noodles or whole grains.
- 2.Increase protein intake to maintain muscle and reduce hunger.
- 3.Exercise regularly (150 minutes/week of moderate activity).
- 4.Monitor blood sugar and weight.
Conclusion
Diabetes is a serious global health challenge, but it is not inevitable. By making smart food choices, especially incorporating Konjac noodles and High Protein noodles into daily meals, people can support healthy blood sugar levels, manage weight, and lower the risk of complications.
Healthy eating is not about giving up your favorite dishes — it is about finding better alternatives that protect your future.
Every meal is a chance to fight diabetes. Why not start with a bowl of noodles that loves your health as much as you do?
FAQs
1. Are konjac noodles safe for people with diabetes?
Yes. Konjac noodles are very low in digestible carbohydrates and calories, making them safe for people with diabetes. They do not cause significant spikes in blood sugar levels.
2. How do konjac noodles help control blood sugar?
Konjac contains glucomannan, a soluble fiber that slows down digestion and sugar absorption. This helps stabilize blood sugar and reduce post-meal spikes.
3. Can konjac noodles help with weight management?
Yes. Konjac noodles are filling but very low in calories. They increase satiety, making it easier to reduce overall calorie intake, which is important for weight control in diabetes.
4. Do konjac noodles have any protein?
No, konjac noodles are almost pure fiber and water, with very little protein. That’s why it’s a good idea to combine them with protein-rich foods (like eggs, lean meat, tofu, or high-protein noodles).
5. Will eating konjac noodles replace my diabetes medication?
No. Konjac noodles can support healthy eating but should not replace prescribed medication or medical advice. They are a complementary part of a balanced diabetes-friendly diet.
6. Are there any side effects of eating konjac noodles?
Some people may experience bloating, gas, or mild digestive discomfort if they eat too much fiber suddenly. It’s best to start with small portions and drink enough water.
7. How often can people with type 2 diabetes eat konjac noodles?
They can be eaten daily as part of a balanced diet, especially when used to replace high-carb foods like regular pasta or white rice.
8. What’s the difference between konjac noodles and high-protein noodles for diabetes?
Konjac noodles: Very low in calories and carbs, but low in protein. Best for lowering blood sugar and calorie intake.
High-protein noodles: Moderate carbs, higher protein. Better for satiety, muscle health, and blood sugar control when paired with exercise.
9. Can konjac noodles lower cholesterol too?
Yes. Studies have shown that glucomannan fiber may help reduce LDL cholesterol and improve lipid profiles, which is beneficial for people with diabetes who are at higher risk of heart disease.
10. How can I prepare konjac noodles for a diabetes-friendly meal?
Rinse them well, then stir-fry or boil. Combine with lean proteins, healthy fats (like olive oil), and non-starchy vegetables for a balanced, blood sugar-friendly dish.






